Featured
Portrait of a Broken Heart: Race-based Stress – A Holocaust from Within

Nearly half of America’s black men and women over 40 have some form of heart disease, (49% and 46% respectively). The businesses of Western Medicine and Weight-Loss, two multi-billion dollar industries, would have you believe this is a consequence of the high-fat, calorie-dense “southern diet.” While there are certainly negative cardiovascular consequences attributable to the southern diet, southern whites do not experience the same degrees of cardiovascular disease as blacks. Thus, presuming black America’s cardiac concerns are completely dietary-driven is sloppy science at best. Hypertension is the gateway to cardiovascular problems. Hypertension is common among U.S. blacks. Western medicine also presumes that blacks have a genetic predisposition to hypertension that is peculiar to sub-Saharan Africans.
 The Department of Genetics at Harvard University explored the latter notion with a meticulous racial admixture study of over 1200 people and determined there is no genetic connection between African ancestry and hypertension. The World Health Organization conducted a longitudinal study of hypertension in three populations: sub-Saharan African blacks, Caribbean blacks, and U.S. blacks. They found a very clear gradient: sub-Saharan African blacks had the least hypertension (actually lower percentages than Europeans and American whites) Caribbean blacks reported slightly higher incident of hypertension, and as all expected hypertension among American blacks was through the roof.
The Department of Genetics at Harvard University explored the latter notion with a meticulous racial admixture study of over 1200 people and determined there is no genetic connection between African ancestry and hypertension. The World Health Organization conducted a longitudinal study of hypertension in three populations: sub-Saharan African blacks, Caribbean blacks, and U.S. blacks. They found a very clear gradient: sub-Saharan African blacks had the least hypertension (actually lower percentages than Europeans and American whites) Caribbean blacks reported slightly higher incident of hypertension, and as all expected hypertension among American blacks was through the roof.
 Robert Sapolsky, a brilliant Stanford neuroscientist, and The Whitehall Studies in London put the final nails in the coffin of Western Medicine’s conceit towards black American heart health. Sapolsky discovered a direct correlation between social rank and stress in baboons. Baboon society is hierarchal, like human society. Baboons on the lower rungs had higher biological stress markers than the alpha male baboons and their mates. Meanwhile, in London, The Whitehall Studies investigated social determinants of health in nearly 30,000 British civil service workers in a cohort investigation over a ten-year span. They found that the lowest level employees had a mortality rate three times higher than those at the highest level did. They also had more hypertension, cardiovascular disease, obesity, and substance abuse issues. This dynamic sounds familiar, oh yeah—it is a snapshot of black America’s declining health status.
Robert Sapolsky, a brilliant Stanford neuroscientist, and The Whitehall Studies in London put the final nails in the coffin of Western Medicine’s conceit towards black American heart health. Sapolsky discovered a direct correlation between social rank and stress in baboons. Baboon society is hierarchal, like human society. Baboons on the lower rungs had higher biological stress markers than the alpha male baboons and their mates. Meanwhile, in London, The Whitehall Studies investigated social determinants of health in nearly 30,000 British civil service workers in a cohort investigation over a ten-year span. They found that the lowest level employees had a mortality rate three times higher than those at the highest level did. They also had more hypertension, cardiovascular disease, obesity, and substance abuse issues. This dynamic sounds familiar, oh yeah—it is a snapshot of black America’s declining health status.
Let us connect the dots. Diet may contribute to cardiac health issues among American blacks, but it is not the source of the problem. It is not genetic and American blacks have higher hypertension than any other blacks on earth. Lower social rank elevates biological stress markers in humanlike primates. Lower level employees have mortality rates that are three times higher than upper level workers, and much worse health outcomes. These are the dots: social rank equals stress in the body; social rank equals negative health outcomes.

 Now, add this piece to the puzzle: the negative health outcomes that black America is experiencing transcends socio-economic status because not all blacks reside in the lower economic, professional or educational ranks, yet statistically all American blacks experience the same health disparities. Is there a common stressor that is unique to black Americans regardless of income, social status, or education? Of course there is. Black America ubiquitously endures the continuous assault of race-based stress, from the most socially disenfranchised black person to the First Family. America is primarily a pigmentocracy. Race-based stress is serious. Race-based stress has the biological authority to sign black America’s death warrant. As hyperbolic as that sounds, it is not. Race-based stress is as serious as a heart attack because it is the source of black America’s cardiac, as well as many other concerns.
Now, add this piece to the puzzle: the negative health outcomes that black America is experiencing transcends socio-economic status because not all blacks reside in the lower economic, professional or educational ranks, yet statistically all American blacks experience the same health disparities. Is there a common stressor that is unique to black Americans regardless of income, social status, or education? Of course there is. Black America ubiquitously endures the continuous assault of race-based stress, from the most socially disenfranchised black person to the First Family. America is primarily a pigmentocracy. Race-based stress is serious. Race-based stress has the biological authority to sign black America’s death warrant. As hyperbolic as that sounds, it is not. Race-based stress is as serious as a heart attack because it is the source of black America’s cardiac, as well as many other concerns.
 First, you need to remember that unlike human society and technology, which has changed at a lightening pace, evolutionary human biology has remained static. While technology has created social media and we are tweeting like birds, biologically speaking, we are still in the wild trying to capture birds to eat.
First, you need to remember that unlike human society and technology, which has changed at a lightening pace, evolutionary human biology has remained static. While technology has created social media and we are tweeting like birds, biologically speaking, we are still in the wild trying to capture birds to eat.
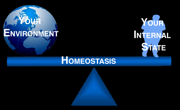
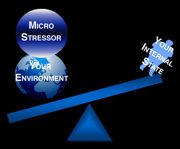
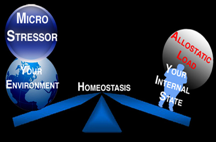
Second, you need to under stand the key components of stress science. Here is a simple explanation of the internal milieu, external milieu, homeostasis, allostasis, and allostatic load. Simply put the internal milieu is the internal environment, and the external milieu the external environment. Homeostasis is the body’s ability to physiologically regulate its inner environment to ensure its stability in response to fluctuations in the external environment. Allostasis is the process humans use to bring the internal milieu back to homeostasis. Allostatic load occurs when the physiological mechanisms used in allostatic processes are over-exerted, causing them to go from making you healthy to making you sick.
Stress and the Brain
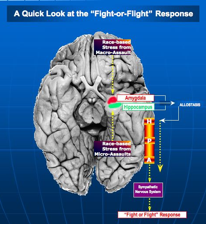 Any intrusion on the homeostasis of an organism requiring allostasis to restore equilibrium is stress. The brain is the key organ in the allostatic response mechanisms that mediate stress. The brain determines what is threatening and potentially stressful based on emotion, learning and memory. The hippocampus is the brain’s primary memory center. It acts as monitor of reality. It compares the outside world with the brain’s representations of how it should be, based on experience, learning and memory. When your world is not how it should be, stress or threat occurs. The hippocampus notifies the Amygdala, which is like brain’s head of security. The Amygdala sounds the “incoming-stress-homeostasis-disrupted” alarm; begin allostasis.
Any intrusion on the homeostasis of an organism requiring allostasis to restore equilibrium is stress. The brain is the key organ in the allostatic response mechanisms that mediate stress. The brain determines what is threatening and potentially stressful based on emotion, learning and memory. The hippocampus is the brain’s primary memory center. It acts as monitor of reality. It compares the outside world with the brain’s representations of how it should be, based on experience, learning and memory. When your world is not how it should be, stress or threat occurs. The hippocampus notifies the Amygdala, which is like brain’s head of security. The Amygdala sounds the “incoming-stress-homeostasis-disrupted” alarm; begin allostasis.
Allostasis
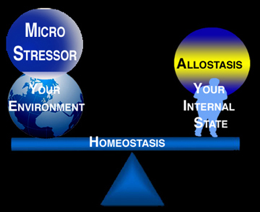 While Allostasis sounds like a medieval pope or obscure rapper, it is actually the body’s physiological and behavioral responses to threat and stress. The operational function of allostasis is to make energy earmarked for long-term usage accessible for immediate needs. Allostasis begins in the hypothalamus. The hypothalamus alerts the adrenal glands, which are on top of the kidneys. The adrenals respond by pouring out the first stress hormones. Epinephrine (adrenaline) enacts the classic fight or flight response, increasing heart rate and raising blood pressure, sending extra blood to the muscles and organs to prepare for the eventuality of fight or flight. Bronchial tubes in the lungs dilate sending more oxygen to the brain, triggering fibrinogen, which accelerates blood clotting a further defense against blood loss e.g., from the infliction of wounds. These events mobilize the body to release glucose from energy stores such as glycogen, and to release fatty acids from stored fats to provide a ready source of energy.
While Allostasis sounds like a medieval pope or obscure rapper, it is actually the body’s physiological and behavioral responses to threat and stress. The operational function of allostasis is to make energy earmarked for long-term usage accessible for immediate needs. Allostasis begins in the hypothalamus. The hypothalamus alerts the adrenal glands, which are on top of the kidneys. The adrenals respond by pouring out the first stress hormones. Epinephrine (adrenaline) enacts the classic fight or flight response, increasing heart rate and raising blood pressure, sending extra blood to the muscles and organs to prepare for the eventuality of fight or flight. Bronchial tubes in the lungs dilate sending more oxygen to the brain, triggering fibrinogen, which accelerates blood clotting a further defense against blood loss e.g., from the infliction of wounds. These events mobilize the body to release glucose from energy stores such as glycogen, and to release fatty acids from stored fats to provide a ready source of energy.
Allostatic Load:
 Allostatic Load describes the biological consequences of excessive stress. It occurs when the allostatic response mechanisms of the body, which keep you healthy, start making you sick from overuse. The sudden surges in blood pressure and accelerated heart rates allostasis uses to carry oxygen to the large limbs to prepare for fight or flight become hypertension, atherosclerosis and irregular heart rhythms when you are in allostatic load. Allostasis’ necessary mobilization of glycogens for quick energy becomes diabetes. Cortisol levels that report the presence or absence of threat in allostasis become the inability to habituate and you get that person that just cannot let go of something in a reasonably timely fashion.
Allostatic Load describes the biological consequences of excessive stress. It occurs when the allostatic response mechanisms of the body, which keep you healthy, start making you sick from overuse. The sudden surges in blood pressure and accelerated heart rates allostasis uses to carry oxygen to the large limbs to prepare for fight or flight become hypertension, atherosclerosis and irregular heart rhythms when you are in allostatic load. Allostasis’ necessary mobilization of glycogens for quick energy becomes diabetes. Cortisol levels that report the presence or absence of threat in allostasis become the inability to habituate and you get that person that just cannot let go of something in a reasonably timely fashion.
The Brain and Race-Based Stress
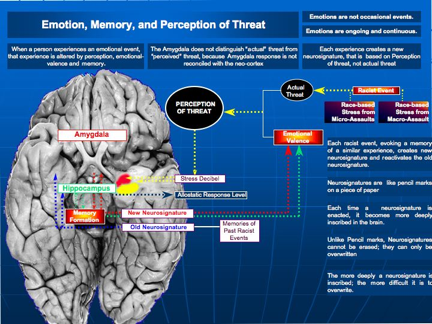
Here is the problem. The brain structures that launch the stress /threat response in the brain are subcortical structures in the old mammal brain. It is all about “survive now and ask questions later.” Thinking is a cortical enterprise, so thinking does not occur in the brain region responsible for launching the stress response. Nor can it distinguish between perceived and actual threat. It is why the Zebra will always run from a rustle in bushes. Likewise, when an African American experiences a racial micro-stressor, e.g., a woman clutches her purse as a black man walks by, the barrage of racist assaults on the Obama’s, the intrinsic racism in the language, i.e., all that is bad is dark or black, all that is good or pure is light or white. The old mammal brain processes these constant micro-stressors like any other threat in the brain, even though they are minor because the old mammal brain does not distinguish between minor and major when it launches the stress response. After the stress response launches, the cortex goes back online and renders input, and we have the advantage of thought. This is why you do not respond to every minor racist assault by attacking or running away screaming.
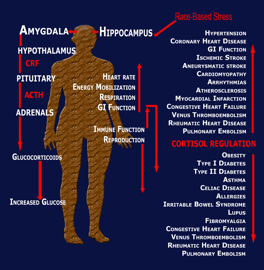 However, on a neurochemical level Elvis has already left the building. Your blood pressure has already risen, your glycogens have already started to break down and your cortisol has risen. This continuous neurochemical drama and the physiological sequelae it inspires is why black America has high blood pressure, prone to diabetes, asthma, and obesity. It is not coincidental that African-Americans have higher rates Cardiovascular, metabolic and inflammatory disorders, which are associated with markers of allostatic-load such as the chronic up-regulation of cortisol and corticotrophin releasing factor (CRF).
However, on a neurochemical level Elvis has already left the building. Your blood pressure has already risen, your glycogens have already started to break down and your cortisol has risen. This continuous neurochemical drama and the physiological sequelae it inspires is why black America has high blood pressure, prone to diabetes, asthma, and obesity. It is not coincidental that African-Americans have higher rates Cardiovascular, metabolic and inflammatory disorders, which are associated with markers of allostatic-load such as the chronic up-regulation of cortisol and corticotrophin releasing factor (CRF).
Black America has faced the threat of genocide since the first African slaves arrived at Jamestown. History removed the chains of our ancestors, but the eminent threat of genocide is stronger than ever. Unlike the 1700’s when the foe had a face, a name, and a clearly defined agenda, the current enemy has none of those and hence more lethal and likely to prevail because of it. Hippocrates said, “the ability of a disease to do damage lies in its ability to remain undetected.” Like the line between love and hate, in medicine the line between detected and diagnosed is thin and separates too very different realities. Sadly, cardiovascular, inflammatory and metabolic disease in black America is an example of this.
Dr. Billi Gordon’s Bio
Think of the most interesting man you know. Now imagine what he would be like had he grown up in a tarpaper shack without indoor plumbing, in a small town called Dowagiac Michigan, which is about 20 miles north of the University of Notre Dame. Imagine if he had joined a monastery, had an extensive career as a female model, actress, author and screen writer, then traded in his weave and acrylic nails for a Ph.D. in neuroscience. If you have been able to conjure up that image, turn it up to 11, then introduce yourself to Dr. Billi Gordon.
Whether you know it or not, if you were born prior to 1980, you have probably seen “Billi” before — if not in Coming to America, or on Married With Children, then most likely gracing the cover of a greeting card featuring a voluptuous black woman inviting you to do something lewd on your birthday. Or perhaps you have seen him on Billboards in the European Commonwealth or in Japanese Commercials. Yep, that was Billi Gordon.
These days, Dr. Gordon spends most of his time conducting research using functional magnetic resonance imaging (fMRI) to identify the neurological basis of behavior. In particular, he studies the pathophysiology of stress as an antecedent to disease. His research is driven by the desire to increase awareness and make a kinder more salubrious world.
Education
Dr. Gordon graduated with honors from the University of Michigan, Ann Arbor in 1997, under the mentorship of Dr. Sandra Cole, Professor, University of Michigan School of Medicine. He graduated summa cum laude with an Interdisciplinary Masters in Psychology and Sociology at California State University at Northridge, under the direction of Dr. James Elias, the last active researcher from the original Kinsey Institute, Director of the Center for Sex Research, and Preferred Expert Testimony by the United States Supreme Court in Human Sexuality Matters. In November, 2004, following the conclusion of a 3-year internship at the Brain Mapping Core of the Center for Neurovisceral Sciences and Women’s Health in the Department of Digestive Diseases in the David Geffen School of Medicine at UCLA, Gordon was awarded his Ph.D in Neuroscience. Dr. Gordon did his Post Doctoral Research at the David Geffen School of Medicine at UCLA under the supervision of Mark S. Cohen PhD, in Brain Research and Functional Neuroimaging at the UCLA Brain Mapping Center. During this time, Dr. Gordon served on the Advocacy Committee of UCLA Society of Post Doctoral Scholars.
Professional
Dr. Gordon currently serves as Chair of the Advisory Committee for Collective Concerns in Medicine. He’s a member of SAG-AFTRA and the Writer’s Guild of America, PEN-USA, and has authored Four Books.

-

 Featured12 months ago
Featured12 months agoArkansas Sheriff Who Approved Netflix Series Says He Stayed ‘In His Lane’
-

 HBCUS12 months ago
HBCUS12 months agoSenator Boozman Delivers $15 Million to Construct New UAPB Nursing Building
-

 News12 months ago
News12 months agoMillions In the Path of The Total Solar Eclipse Witnessed Highly Anticipated Celestial Display
-

 Featured9 months ago
Featured9 months agoCalifornia Is the First State to Create A Public Alert for Missing Black Youth
-

 Featured9 months ago
Featured9 months agoAfrican American Leaders Stay the Course Amid Calls for President Biden To Bow Out of Race
-

 Featured9 months ago
Featured9 months agoThe Debate Fallout Lands on Both Candidates

